Thursday, January 9, 2014
Sealant Inspired By Beach Worm Could Become Surgical Superglue
Heck, a version of the everlasting adhesive is even approved by the Food and Drug Administration to seal skin wounds.
But superglue can't fix a broken heart — or even a torn artery. Yet.
Now a team of doctors and engineers at Brigham and Women's Hospital in Boston are getting close to changing that. Their unlikely inspiration is a 3-inch worm that lives off the coast of California.
Cardiac surgeon Pedro del Nido and his colleagues have developed a biodegradable adhesive that can patch a hole in a pig's heart or artery. The experimental glue is nontoxic and is strong enough to hold up under the high pressures in the human heart, the team report Wednesday in the journal Science Translational Medicine.
So far, they've tested the glue only in animals. So the sealant is far from reaching the operating room or battlefield. But del Nido hopes the adhesive will eventually replace traditional sutures and staples for some operations, especially heart surgery.
"A glue is the holy grail for repairing hearts," del Nido tells Shots. "Right now we use sutures. Every time the needle and thread enter normal tissue, they do a little bit of damage. Usually it doesn't matter. But I repair children's hearts. For those, this damage can really be a problem."
Regular superglues don't work well inside the body. "It's a skin glue," del Nido says. "You can't use it internally because it hardens as soon as it comes into contact with water." And the glues are made from a compound called cyanoacrylate, which can be toxic.
To find a safe adhesive that could work on hearts, arteries and other organ surfaces, del Nido teamed up with bioengineer Jeffrey Karp, also at Brigham and Women's Hospital.
"In our lab, we look to nature for inspiration in designing materials," Karp tells Shots. "Solutions are really all around us." Karp's lab has been looking at porcupine quills for insights that could lead to better surgical needles.
The barbs on porcupine quills make it easier from them to penetrate the skin.
For the heart glue, Karp and his team turned their attention to critters that stick to slippery surfaces, such as slugs, spiders and a bristly little worm that glues itself rocks in tidal pools, called thesandcastle worm.
To eat, chitons use their teeth, which look like black bulbs with bluish highlights, to grind up rock.
"We started looking at how creatures, like the sandcastle worm, could attach to wet surfaces," Karp says. After years of experimenting with various chemical cocktails, he and his team finally stumbled upon an adhesive that's biodegradable and nontoxic.
"Cells and tissues can grow over the material and into it," he says. Eventually it just dissolves into the body. And the glue only hardens when UV light shines on it. So a surgeon can put the glue in exactly the right place before it seals up.
Although Karp and del Nido haven't tested the experimental glue on people yet, they've put the adhesive through a whole battery of tests in animals.
"We made a hole in the heart of a living rat and showed that we can seal it up without removing the blood," Karp says. "The animals were fine six months later."
They also patched a pig's heart and carotid artery with the glue. Even after the pig was given a shot of adrenaline and its heart pressure shot through the roof, the patched stayed on the tissue.
Of course, humans are more complicated than pigs and rats. And the glue has to be safe for decades in people, not months.
But Karp is so confident that the adhesive will one day reach surgeon's toolbox that he has procured $11 million to start a company to manufacture and test the glue. "It appears that the glue is safe," he says. "But we do need to do more studies. We'll repeat the animal tests and then move forward in humans."
Monday, October 25, 2010
Study shows use of superglue in chest surgery cuts recovery time in half
 Victor Haddad used Krazy Glue in his woodworking shop for years to mend his accidental wounds. Then last year, as he awaited a heart operation, he discovered on the Internet that a Calgary doctor was using a superglue to fuse bones together after chest surgeries.
Victor Haddad used Krazy Glue in his woodworking shop for years to mend his accidental wounds. Then last year, as he awaited a heart operation, he discovered on the Internet that a Calgary doctor was using a superglue to fuse bones together after chest surgeries.The minute he read about the experimental procedure, he says, “I wanted it.”
He became a patient of Paul Fedak, a cardiac surgeon who pioneered the technique in 2009 at Calgary’s Foothills Hospital Medical Centre. In June of this year, Dr. Fedak replaced Mr. Haddad’s aortic valve and joined his sternum using steel wire, and then sealed the bones with a sticky paste called Kryptonite.
Mr. Haddad was out of the hospital in seven days. Within six weeks, the 59-year-old resident of Milk River, Alta., was back to work as a real-estate broker. Mr. Haddad didn’t bother to fill his prescription for pain meds, he says. “I’ve been pain free since before I left hospital.”
His surgery was standard except that Dr. Fedak took a few minutes to apply adhesive to the ends of the chest bones before stitching up the soft tissue. According to Dr. Fedak, breastbones heal much faster when secured with wire as well as Kryptonite glue.
Instead of it taking six to eight weeks for the bone to fuse back together, “we do it in 24 hours.” The glue makes it rock solid within a day.
A study released Sunday suggests the use of adhesive in chest surgery reduces the normal recovery time by half. Patients have less physical disability in the first six weeks after surgery and can breathe deeply sooner, Dr. Fedak reports. He adds that patients are able to cough with less discomfort and require significantly less medication such as narcotics to manage pain.
No complications or side effects from the glue were reported among the 55 patients in the randomized controlled trial.
The procedure has the potential to improve post-operative care for an estimated 1.4 million open-chest surgeries performed worldwide each year, according to the Heart and Stroke Foundation of Canada.
Dr. Fedak has applied to the Canadian Institutes of Health Research to fund a larger clinical trial involving 2,000 patients throughout North America, which should start in six months, he says.
Although medical adhesives are widely used in hip replacements and other procedures, most bone cements contain toxic ingredients that are dangerous for use in the chest, notes Dr. Fedak. In contrast, Kryptonite is an adhesive polymer composed of calcium carbonate and fatty acids derived from castor bean oil. It is “bio-compatible” and turns into a porous bonelike substance as it cures, he says.
Dr. Fedak doesn’t recommend the adhesive for patients at high risk for internal bleeding and other complications after surgery, because doctors might need to re-enter the breastbone and the procedure would take longer if the breastbone is well-bonded. Otherwise, he says, “you could use this on almost any patient.”
Regulators in Canada and the United States have approved the use of Kryptonite, which is made by the Doctors Research Group in the United States.
The glue is expensive, adding $700 to $1,000 to the cost of performing surgery. The need for public funding is a barrier to routine use, Dr. Fedak says. But he suggests that using Kryptonite could result in net savings to the health-care system by reducing recovery time and major post-op complications, including breastbones that separate after surgery.
“If a patient leaves the hospital a day early, that would be thousands of dollars of savings,” he points out.
Patients from around the world have contacted him, seeking repairs to sternums that didn’t heal properly after surgery, Dr. Fedak says. Although he is cautious about expanding the use of Kryptonite prematurely, he adds, reconstructions to damaged sternums “work very well.”
Mr. Haddad says he’s been the envy of his friends since he was glued back together with Kryptonite. He mentions a neighbour who took more than six months to bounce back after recent heart surgery.
“He is absolutely annoyed that he wasn’t in the [Kryptonite] study.”
Tuesday, August 31, 2010
Oyster glue's secret ingredient
The natural cement produced by oysters to build extensive reef systems contains significantly more inorganic material than the glues of other marine species, and could spur development of new synthetic adhesives for biomedical devices or antifouling coatings for ships, say researchers in the US.
Jonathan Wilker and his team at Purdue University and colleagues at the University of South Carolina have been investigating how oysters bind to reefs and each other, in a bid to develop synthetic composite materials with properties that imitate the oyster glue.
The team analysed the chemical composition of oysters' adhesive using infrared spectroscopy, electron paramagnetic resonance spectroscopy and thermogravimetric analysis. They found higher protein content in the adhesive material than in oyster shell (10 per cent as opposed to 2 per cent), and evidence of protein cross-linking, iron species and radical species.
Sunday, April 11, 2010
Concerns Raised About Synthetic Glue for Hernia Repair
The study, in 16 rats, found that in all cases, the glue prevented tissue from adhering to or integrating with the mesh, impaired tissue flexibility and resulted in a severe inflammatory response marked by large seroma formations.
The cyanoacrylate examined in the study was Glubran 2, made by the Italian firm GEM S.r.l. (Viareggio, Italy) and approved for use in Europe in both traditional and laparoscopic surgery.
“It seems not very appropriate for hernia repair in an experimental model, to say the least,” said the lead author of the study, Alexander H. Petter-Puchner, MD, a surgical resident at the Ludwig Boltzmann Institute for Experimental and Clinical Traumatology in Vienna, Austria.
Surgeons who heard the report said it comes amid a welcomed stream of studies into novel means for fixing mesh during hernia repair.
“There are a bunch of these cyanoacrylates that have been used clinically or investigationally as tissue adhesives,” said Raymond J. Lanzafame, MD, the immediate past president of the Society of Laparoendoscopic Surgeons. “The good news is that some of the the cyanoacrylate compounds are hydrophilic. But they, like the currently available cyanoacrylates, do generate a pretty intense inflammatory response. If it’s a version that isn’t broken down by the body in some way, it can turn out as bad as, if not worse than, a suture granuloma in terms of producing pain and irritation.”
Phillip Shadduck, MD, of Regional Surgical Associates in Durham, N.C., said in an interview after Dr. Petter-Puchner’s presentation that while a strong inflammatory response was seen in the study, newer cyanoacrylates might not evoke the same reaction. “We’ve learned in the abdomen, and now in the abdominal wall, that the chemistry of the cyanoacrylates makes a big difference in the inflammatory response it activates,” he said. “There are newer cyanoacrylates coming out in an effort to elicit less of an inflammatory response.”
One such cyanoacrylate, designed to be biodegradable, was approved for use in Europe in February 2005 as an adjunct to sutures during peripheral vascular reconstructions. The product, Omnex, is made by Closure Medical Corporation in Raleigh, N.C., which was recently acquired by Johnson & Johnson. (Dr. Shadduck reported that he has done consulting on the Omnex product.)
In March at the annual meeting of the Society for Clinical Vascular Surgery, results from a trial of 150 patients at 15 centers in the United States and Europe showed significant benefits for Omnex as an adjunctive sealant for vascular anastomoses compared with Surgicel Nu-Knit Absorbable Hemostat (Johnson & Johnson). The study found a statistically significant difference in time to hemostasis between the sealant, with a mean of 119.3 seconds, compared with Surgicel, with a mean of 403.8 seconds (P<0.001). Among patients in the Omnex group, 54.5% had immediate hemostasis, compared with only 10% in the Surgicel group (P<0.001). No significant difference in incidence of adverse events occurred between the two groups (P=0.60).
Using a compound similar to the one approved for external use in the United States under the trade name Dermabond, Omnex is under consideration by the FDA for internal use during vascular surgery.
Whether Omnex would have the kind of detrimental effects in hernia repair that were seen in Dr. Petter-Puchner’s study of Glubran 2 is unclear, but the chief of minimally invasive surgery at the department of surgery, Keck School of Medicine of USC, Los Angeles, said he would be “wary” of such a use.
“The artificial glues, or glues that have any artificial nature, stay around in the body and create a foreign body reaction,” said Namir Katkhouda, MD, who published the first study using a fibrin sealant, Tisseel, for mesh fixation in hernia repair (Ann Surg2001;233:18-25). “Some people have spun around the concept of using sealants in mesh fixation to these other adhesives [with artificial components]. I am absolutely wary of them. The important difference between the fibrin sealants and any artificial sealant is that the fibrin is naturally removed by the body at 10 days. That’s what you want.”
Tisseel, made by Baxter (Irvine, Calif.), is widely used in Europe for mesh fixation, but is currently approved in the United States only for cardiopulmonary bypass surgery, splenic repair and colostomy closure. A spokesman for Baxter said the company has a “strong desire” to broaden the indications for Tisseel in the United States.
In his award-winning paper, Dr. Petter-Puchner presented data on 20 Sprague Dawley rats, in which two defects per animal were created in the abdominal wall left and right of the linea alba (1.5 cm in diameter), with the peritoneum was spared. The lesions were left untreated for 10 days to achieve a chronic condition and then were covered with 2 cm×2 cm of mesh sealed with Glubran 2. Four of the animals were sacrificed after 17 days, eight after four weeks and another eight after 12 weeks. The meshes were then biomechanically tested and histology was performed.
At the 12-week mark, the hook-pull test revealed a loss of mesh adhesion wherever the sealant had been used. “There was no tissue integration through the mesh and histology revealed strong inflammation,” Dr. Petter-Puchner said during his presentation. “We also saw a huge seroma formation.”
Using a suction cone to test the elasticity of the tissue, his group found 4.2 mm of deformation in untreated areas, but just one-tenth that much in areas where Glubran had been applied, demonstrating a loss of flexibility.
Thursday, August 27, 2009
Sea Worm Provides Model for Surgical Adhesive
Scientists at the University of Utah have uncovered a way to produce a synthetic adhesive based on a natural glue created by the sandcastle worm. This ocean worm builds its home by sticking pieces of sand and shells together, and the result is strong enough to withstand ocean tides. Researchers think this glue could have applications for bone repair in trauma cases, where fast setting time, ease of use and low risk of infection can benefit both the patient and the surgeon.
Russell Stewart, Ph.D., who led the Utah team, said his goal was to develop a water-based adhesive that remained insoluble in wet environments and was able to bond to wet objects. Curing time was another key issue for Stewart. The the team learned that pH changes cause the glue to set, a response that was copied for the synthetic version. The final result is "at least as strong as Super Glue" and is twice as strong as the sandcastle adhesive. So far, it has passed toxicity studies in cell cultures. In addition to its adhesive applications, Stewart is exploring how the glue could also be used to deliver antibiotics or materials that could aid in healing, like BMPs or other small molecules.
Surgical adhesives offer a number of benefits over fixation devices, among them more effective wound closure, less risk of leakage and infection and ease of handling and application. Similar to the sandcastle glue, many adhesives are derived from natural sources. For example, fibrin sealants are blood-derived, CryoLife's BioGlue is bovine-derived and some hemostatic products come from snake venom.
Saturday, July 11, 2009
Glues tailored to specific tissues
Surgical adhesives, which can be used to seal tissues after an operation or to repair wounds, are becoming increasingly important parts of a doctor's toolkit. However, their one-size-fits-all nature means that existing adhesives, or glues, work well in some cases but not in others.
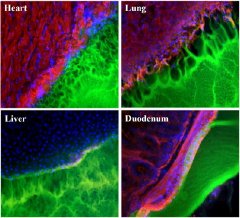 |
| Images showing the interface between a surgical glue (green) and tissue samples (red, blue and black) from the heart, lung, liver, and duodenum. The glue works best with duodenum tissue (note smooth interface), and worst with lung tissue (pockmarked with holes). |
MIT researchers aim to change that with glues tailored to specific tissues. In a recent issue of Advanced Materials, they identified for the first time how one kind of glue material bonds to tissue and how that adhesion varies depending on the tissue involved, from the intestine to the lung. They then showed how by adjusting certain properties of the materials it was possible to create a range of adhesives optimized for specific tissues and applications.
"The delineation of tissue-specific mechanisms for material adhesion leads the way for tailoring materials to individual needs and applications. This exciting work may well change the clinical use and continued evolution of soft-tissue sealants and adhesive materials," said Elazer R. Edelman, principal investigator and MIT's Thomas D. and Virginia W. Cabot Professor of Health Sciences and Technology.
Adhesive sealants could improve patient care and reduce healthcare costs by cutting medical complications after surgery, such as leakage through incisions, and improved wound healing, according to Natalie Artzi, a postdoctoral associate who led the research in Edelman's lab.
Although there is already a billion-dollar market for such adhesives, "they haven't reached their true potential," Artzi said. Existing materials have limitations that often force doctors to compromise between adhesion strength and tissue reaction. For example, said Artzi, for a given tissue, the material may be adhesive but release toxins that could affect healing. Alternatively, the material could be quite tissue compatible, but degrade quickly, becoming non-adhesive. If the glue doesn't work, a doctor must switch to sutures or staples.
The problem, according to the MIT team is that while surgical adhesives rely on intimate interactions between the adhesive and the tissue in question, the properties of the target tissue have been largely ignored in designing adhesives. Instead, "one general formulation is proposed for application to the full range of soft tissues across diverse clinical applications," Artzi and colleagues wrote in their Advanced Materials paper.
The new work characterized a variety of interactions between one kind of glue (hyrogels composed of polyethylene glycol and dextran aldehyde, or PEG: dextran for short) and tissue from a rat's heart, lung, liver and duodenum (the first section of the intestine). The team found, for example, that the glue worked well with tissue from the duodenum, but poorly with that from the lung.
They then went on to "identify the functional groups in the material that are responsible for adhesion with tissue functional groups, and created a model to optimize adhesion for each tissue," Artzi said. In particular the paper explains how variation of chemical reactive groups in the material could be matched to the variability in the density of respective reactive groups on different tissues to regulate tissue-material interaction.
The team will use these findings to "develop a platform of adhesive materials" for specific tissues. Although it could take three to five years before the work translates into a product, "the concept is there," she concluded.
In addition to Edelman and Artzi, co-authors of the paper are Tarek Shazly (co-first author with Artzi and a graduate student in MIT's Department of Materials Science and Engineering), Aaron B. Baker (a postdoctoral associate in Edelman's lab), and Adriana Bon, now at the Universitat Ramon Llull (Spain).
The work was supported by the MIT-DuPont Alliance and the National Institutes of Health, as well as the Philip Morris External Research Program.
Wednesday, March 18, 2009
Researchers hope to take a lesson from mussels

The bandages of the future may come from oceanic tidal zones, where creatures who want to stay in one place have developed sophisticated ways of sticking to things. Frustrated by the inadequacies of human-engineered medical adhesives, researchers hope to take a lesson from mussels, barnacles, tubeworms and other animals that can resist the ocean's buffeting currents. "The interface between ocean and land has been an important zone in evolutionary history," said University of Utah biochemist Russell Stewart. "Marine organisms exploit multiple bonding mechanisms. By using multiple chemical bonds, they're able to bond to multiple substrates" — a fancy way of saying they can stick to anything. Chemists recently made prototype bandages with an inkjet printer filled with adhesive proteins taken from mussels, whose remarkable "feet" — a tangle of fibers that anchor them to rocks — have made them the most widely-studied specialist in marine clinging. Mussels can also attach themselves to wood, iron, steel, each other, and even Teflon. The shortcomings of modern medical adhesives are manifold. As anyone who's ever put a Band-Aid on an elbow knows, off-the-shelf medical glues aren't suitable for moving joints. Sutures — which can be thought of as a form of mechanical adhesion — can leave scars and leave bodies open to infection. Sealants made from blood-coagulating compounds are promising, but still prone to contamination. And surgical-grade glues are essentially Krazy Glue with different brand names. As the instructions on Krazy Glue packets make clear, it's a toxic substance not meant to be put inside a body, even if it could seal a tissue under repair by a surgeon — which, often, it can't. The inside of a body, however, poses many of the same challenges as an intertidal zone. Marine glues need to stick to wet surfaces. They do so by employing a variety of chemical bonds to displace the water, right down to the last molecule. Then they need to keep their glue from dissolving in water. "There are chemical changes and cellular changes within the body, and all sorts of causes" that can dissolve a medical adhesive, said University of North Carolina bioengineer Roger Narayan, coauthor of the inkjet adhesive study in the Journal of Biomedical Materials Research Tuesday. Earlier research by co-author Jonathan Wilker, a chemist at Purdue University, showed that mussels strengthen their glue with molecules of iron, though the mechanical details of this process remain unclear. So do the molecular details of mussel adhesive itself. The glue is made from a mix of proteins that can be harvested and even synthesized — but much of its adhesive power comes from the proteins' structural arrangement. That's lost during harvesting, and can't yet be artificially replicated. "There's a gradient of proteins in that structure," said Stewart. "The proteins have different functions: varnishes, primers, the parts that connect the adhesive" to the threads that compose the mussel's foot. The difficulty in recreating mussel protein structures could explain why mussel-based medical adhesives are not yet on the market, despite nearly two decades of research. Stewart has chosen a less-complicated source of inspiration: the polycheate, a surf-dwelling worm that glues together grains of sand to make a tubular home for itself. "The mussel has to glue a string to a wet rock, whereas a polycheate just has to glue two similar materials together. That's a much simpler bonding problem," said Stewart. At the point of contact between surface and adhesive, said Stewart, polycheate and mussel glues — though composed of similar proteins — likely rely on a different mix of molecular bonds. Among them are the van der Waal forces of gecko foot fame, hydrogen bonds, covalent bonds, and salt bridges — a smorgasbord of molecular stickiness. The bonds have been identified, said Stewart, but not their configuration, or their relationship to individual proteins. Researchers need to determine "the proportion of different bonds, and how those might work in some cooperative and unexpected manner." Meanwhile, barnacles — the least-understood marine adhesive — don't use dopa, a protein central essential for mussel and polycheate glues. The lack of dopa, said Stewart, shows just how many ways nature has found to solve the problem of adherence in the surf. "A lot of these things are not well-understood," said Narayan. "These sorts of studies are the first steps to better understanding these materials."
Wednesday, November 12, 2008
Natures Superglue
 How does an aquatic bacterium that colonizes streams, rivers, and water pipes resist being swept away by a forceful current or running tap water? The answer lies in a bacterially-produced, secreted substance, consisting of polysaccharides (long chains of sugar molecules) along with other unidentified sticky molecules, on the "holdfast" at the tip of its long, slender, stalk-like appendage, with which it affixes itself to solid surfaces.
How does an aquatic bacterium that colonizes streams, rivers, and water pipes resist being swept away by a forceful current or running tap water? The answer lies in a bacterially-produced, secreted substance, consisting of polysaccharides (long chains of sugar molecules) along with other unidentified sticky molecules, on the "holdfast" at the tip of its long, slender, stalk-like appendage, with which it affixes itself to solid surfaces.Professor Yves BrunThe common, hydrophilic bacterial strain Caulobacter crescentus (C. crescentus) is a gram-negative, rod-like bacterium that lives in all sorts of water sources, including lakes, streams, sea water, waste water, and even bottled spring water, attaching itself to solid substrates such as plants, other microorganisms, glass, stone, and metal. Evolution has enabled C. crescentus to live under nutrient-poor conditions, hence its ability to exist even in tap water. Producing no human toxins, its presence in drinking water is innocuous to humans.While studying developmental aspects of C. crescentus, Indiana University biologist Yves Brun and lab members discovered that the bacteria could not be removed with strong washing from plastic overhead transparencies. In contrast, they found that their genetically-manipulated C. crescentus mutants, which lacked these sugar molecules at the tip of the stalk, were no longer able to bind to surfaces. In collaboration, Brown University physicist Jay Tang (formerly of Indiana University) and colleagues determined that three times as much force had to be applied to remove a single C. crescentus bacterium from a glass pipette compared with a pipette containing a similar amount of commercial super glue. Furthermore, they measured the physical force required to remove C. crescentus from its affixed glass surface, determining it to be over an incredible 70 N/mm2 (newtons per square millimeter; about 5 tons/in2), equivalent to the downward force exerted by three cars balancing on a quarter.
This natural, non-toxic glue, which can be found in small quantities in drinking water, has the strongest adhesion force of any known natural material. Unlike commercial super glues, which are often toxic, it sticks well under water, even salt water, and, thus, has a wide range of potential applications, from biodegradable surgical or dental adhesives to repairing industrial surfaces that suffer rain or sea exposure.

